NORD supports the ability of rare disease patients to access comprehensive health care services through expanded financial eligibility for Medicaid
Medicaid is an entitlement program administered through a partnership between the federal government and state governments, wherein individuals who meet certain criteria are provided with access to no cost or low-cost health care services. However, each state has a significant role in shaping its own Medicaid program, resulting in considerable variability in program eligibility and benefits.
Medicaid plays an important role in supporting the rare disease community, as many individuals with rare diseases depend on Medicaid for primary or supplemental health care coverage. As of August 2023, Medicaid covers more than 83 million Americans, making it the largest provider of health care coverage in the United States and a critical safety net for its enrollees.1
Medicaid Financial Eligibility
Prior to the enactment of the Affordable Care Act (ACA) in 2010, United States citizens could be eligible for Medicaid coverage in the state in which they resided if they were members of a specific category (e.g., children, parents of dependent children, pregnant people, etc.) and if their income and combined assets fell within a range determined by the state. The ACA amended this eligibility standard by removing the specific categories and establishing a nationwide minimum income eligibility level at 138% of the federal poverty level (FPL) for all states operating Medicaid programs. In 2023, 138% of the FPL for an individual was $20,120.2 This policy is referred to as Medicaid “expansion.”
In 2012, however, the Supreme Court found the ACA’s establishment of a national minimum income eligibility level to be unconstitutional, leaving the decision of whether to expand Medicaid to individual states.3 Since that decision, most states have chosen to expand Medicaid to a minimum eligibility level of 138% of the FPL and provide Medicaid coverage for childless adults, who had prior to the ACA been ineligible for coverage. In these states, expansion has resulted in fewer uninsured Americans and allowed many people with rare diseases to obtain vital health care coverage. Unfortunately, as of December 2023, 10 states have not opted to expand Medicaid, depriving millions of uninsured or underinsured Americans access to quality, affordable health care coverage.4
Children’s Health Insurance Program (CHIP)
Like Medicaid, CHIP is a joint venture between the federal government and state governments in which states can opt to cover children whose families earn incomes above current Medicaid eligibility levels.
Each state determines its upper income limits for CHIP eligibility, resulting in regional variability. The national average of the upper income limit is 255% of the FPL.5 As of August 2023, almost 7 million children were enrolled in CHIP.6
2023 Update on Eligibility Requirements
In December 2023, North Carolina became the latest state to expand their state’s Medicaid program.7 In August 2022, Georgia, a non-expansion state, was given permission by a federal judge to move forward with their “Georgia Pathways” program, offering Medicaid coverage to an estimated 50,000 Georgia residents.8 While this increase in Medicaid eligibility has caused Georgia’s grade in this section to improve, a full expansion of Medicaid would have covered an additional estimated 450,000 Georgians. Georgia is requiring beneficiaries to comply with harmful policies, including a work requirement, in order to maintain coverage. NORD is concerned with this policy decision and opposes programs that implement barriers that would limit a person’s ability to receive quality, accessible health care. For more information on this issue please visit NORD’s Protecting Patients in State Medicaid Programs” section of the Report Card
Medicaid Unwinding
Throughout the COVID-19 pandemic, states were required to continue providing Medicaid services to existing beneficiaries in exchange for increased federal funding. In March 2023, this continuous enrollment provision was terminated and, as a result, states around the country are re-evaluating whether individuals currently covered by Medicaid should retain their coverage moving forward. Each state has implemented a different process for determining continued eligibility. Per KFF, at least 11 million people have been disenrolled as of November 27, 2023.9 NORD is deeply concerned about the extent of coverage losses. Although a state’s procedures related to Medicaid unwinding is not graded as a part of this year’s State Report Card, NORD continues to monitor the situation closely.
Notes on Methodology Changes
This year, the final grade states received are based on an average grade from each of the four reviewed categories: Eligibility for Childless Adults, Eligibility for Parents of a Dependent Child, Eligibility for a Pregnant Person, and Eligibility for Children. Within the Eligibility for Children category, the grade was derived from an average of the four subcategories: Medicaid eligibility for ages 0-1, 1-5, 6-18 and Separate CHIP for children aged 0-18. Although the upper income limits of CHIP programs are often greater than the upper income limits of Medicaid programs, there is a significant difference in the benefits conferred which necessitates an independent category.
Grading Methodology
To evaluate eligibility standards, NORD graded states on each of the following categories:
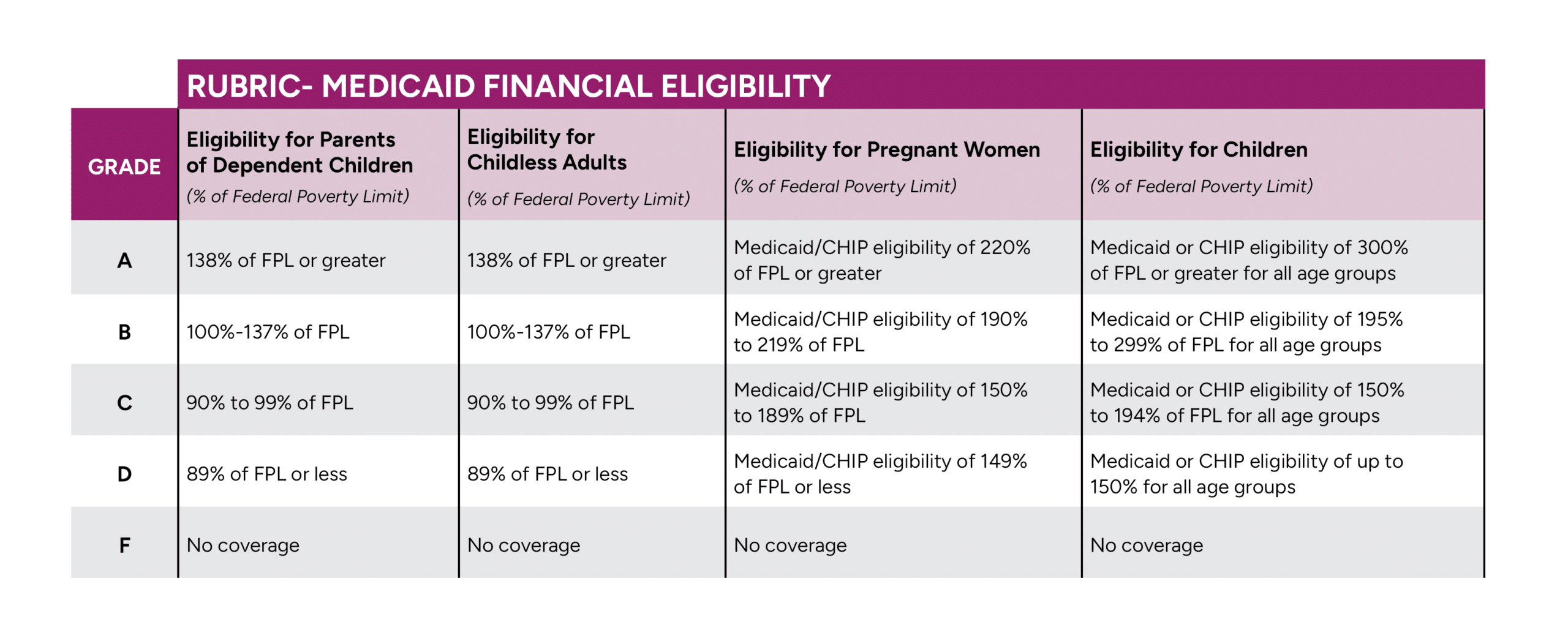
Click to enlarge
Your donation will help more than 30 million Americans with a rare disease navigate their diagnosis, receive financial assistance, and access the care and support they deserve. Make your tax-deductible gift today!